What is the Difference Between Antibody vs. Antigen Testing?
Antigen vs. Antibody Tests
As the COVID-19 pandemic continues to spread in the United States and worldwide, people need answers to questions about their health. If they’re experiencing symptoms or have been in contact with someone contagious, they need reliable ways to determine whether they have become infected. If they believe they may have gotten sick in the past, they must have dependable ways to assess their bodies’ antibody levels.
Continuous testing is a crucial part of responding to the ongoing COVID-19 pandemic. It is essential to understand the differences between antibody and antigen testing and how either can impact your health and that of everyone at your workplace. For instance, what is the COVID-19 antigen test, and what is an antibody test? You also need the information necessary to determine which one is right for your situation.
What Are the Types of Testing for COVID-19?
How are people tested for COVID-19? Below are the available types of tests.
1. PCR Testing
One widely deployed COVID-19 test is polymerase chain reaction testing. A reverse transcription polymerase chain reaction test, also known more briefly as a PCR or a molecular test, detects ribonucleic acid, the virus’ genetic material. If you have gone to a clinic for a COVID-19 test and gotten your results back within the next few days, you’ve almost certainly had a PCR test.
The PCR test usually requires an oropharyngeal or nasopharyngeal swab, though in some cases, it uses saliva. Healthcare workers can then test the sample for antigens. This test’s main drawback is that it requires processing in a medical laboratory and is not available for rapid point-of-care or workplace testing.
PCR testing uses a lab technique known as a polymerase chain reaction to identify nucleic acids. When lab professionals first receive a throat or nasopharyngeal swab, they treat the organic matter with chemical reagents to remove proteins and fats, leaving only nucleic acids behind. They then use an enzyme and reverse transcription processes to build DNA using single RNA strands as templates. They also create short strands of DNA that are complementary to individual segments of the SARS-CoV-2 DNA. These shorter strands will act as marker labels.
Then, the lab professionals place the DNA in the RT-PCR machine, which copies the created DNA hundreds of thousands of times. The copies multiply exponentially — two become four, four become eight, eight become 16 and so on. This extensive copying makes detecting specific viruses easier. At the end of the process, as many as 35 billion copies of the original genetic material may be present.
As copying occurs, some of the shorter DNA segment markers attach themselves to the newly completed strands as the SARS-CoV-2 viral material replicates. They release a fluorescent dye that the machine’s computer can detect and report. Fluorescence indicates viral presence, and how quickly the fluorescence builds up shows how much of the virus is present.
Companies generally do not sell PCR test kits for home or workplace testing. The intensive laboratory requirements for processing make these tests inviable for in-home use.
2. Antigen and Antibody Testing
Two of the main types of COVID-19 tests are antigen and antibody testing. These are the methods SUNLINE sells testing kits for.
- Antigen testing: Antigen testing looks for antigen markers in a swab of your nasal or throat fluids. It detects an active SARS-CoV-2 viral infection in the body. It provides near-immediate results and can occur at a clinic, testing site or workplace or even in the home.
- Antibody testing: Antibody testing, or serology testing, looks for antibodies in the blood serum. It detects previous SARS-CoV-2 viral infections.
What Is the Difference Between an Antigen and an Antibody?
Let’s take a moment to discuss antigens vs. antibodies.
An antigen is a molecule that can elicit a response from the body’s immune system. Like the SARS-CoV-2 virus that causes COVID-19, a virus might consist of different types of antigens that have distinct features when they react to the immune system. An easier way to think of an antigen is to imagine any substance your body does not recognize and tries to fight off.
An antigen often takes the form of a specific chemical structure like these:
- A protein
- A polysaccharide
- A lipid
- A nucleic acid
Each antigen has characteristic surface features the body’s immune system can recognize. SARS-CoV-2 has numerous distinctive antigens – most notably the protrusions on its surface, the glycoproteins. When you look at magnified pictures of the SARS-CoV-2 virus, the very tips of the spiky protrusions you see are the glycoproteins. The nucleocapsid phosphoprotein of the virus’s RNA also acts as an antigen.
When the immune system reacts to an antigen, the body creates antibodies, also known as immunoglobins, to respond to the foreign substance and act to fight it off. These Y-shaped proteins produced by B-lymphocytes act in defense of your immune system to keep foreign substances, like viruses, out of the body. For example, if your body becomes infected with SARS-CoV-2, your immune system creates antibodies specifically to bind with antigens related to the virus to help eliminate them.
The tip of each arm on the Y-shaped antibody protein contains what are known as paratopes, or antigen-binding sites. These sites bind to specific regions, known as epitopes, on the antigen’s surface. This binding action helps remove the antigens from the body. Sometimes an antibody can neutralize and remove antigens directly, or it can mark them for elimination elsewhere in the immune system.
When the body becomes infected with a virus such as SARS-CoV-2, it produces antibodies specifically designed to bind to antigens like the spike proteins and help rid your body of the virus. These antibodies generally remain in the body over the long term to aid in fighting off future infections.
What Is a COVID-19 Antibody Test?
What is an antibody test for COVID-19? A COVID-19 antibody test looks for antibodies in the blood. A binding antibody test may take the form of a laboratory test like a chemiluminescent immunoassay or enzyme-linked immunosorbent assay. It may also sometimes be a quick point-of-care test that uses lateral flow technology.
Unlike the PCR and antigen test, which require swabs or saliva samples, the antibody test requires a blood draw or finger stick. Healthcare professionals then analyze the blood sample for the presence of the relevant IgG and IgM antibodies. Some antibody tests can give same-day results, though others require a few days for processing.
Purchase Antibody Testing Kits Now
The CDC’s serologic test, for instance, tests for antibodies using an ELISA test, deploying purified SARS-CoV-2 S protein as an antigen. These proteins will bind to and indicate any antibodies present in the blood.
What Does an Antibody Test Tell You?
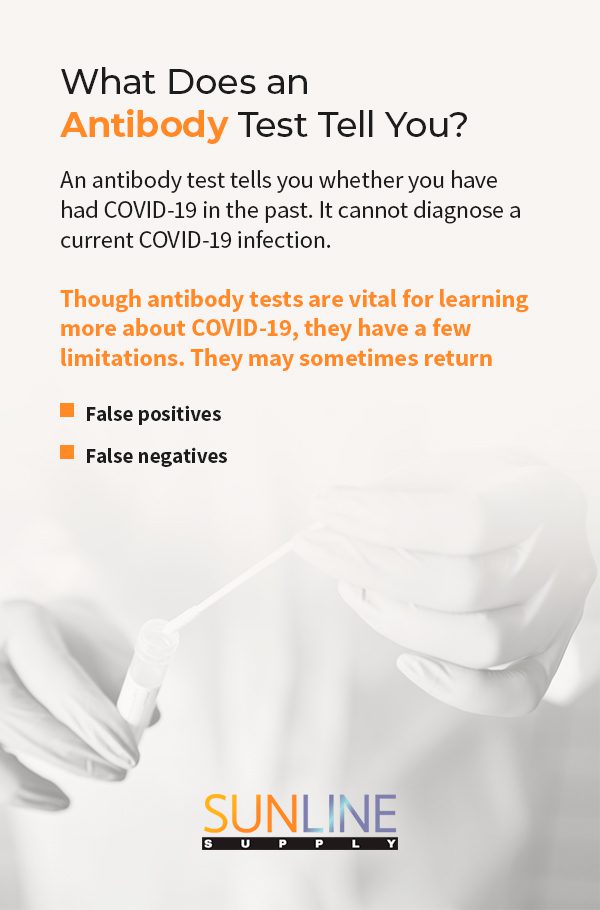
An antibody test tells you whether you have had COVID-19 in the past. It cannot diagnose a current COVID-19 infection.
If you test positive on an antibody test, you may have previously had COVID-19. However, a slight possibility exists that the antibodies come from earlier infections with other viruses in the coronavirus family. Because of the potential for false positives, and because researchers are not yet sure how long post-infection immunity may last, you should continue to wear masks, practice social distancing and use other personal protective equipment at work if necessary.
If you test negative on an antibody test, you most likely have not had COVID-19. You could currently have the virus, and it is also possible to have had an active infection, but never develop antibodies. Still, the most likely scenario is that you have not contracted COVID-19 before.
An antibody test allows healthcare professionals to track the spread of viruses like SARS-CoV-2 and understand who might have already contracted COVID-19, even if they did not show any outward symptoms. Antibody tests also help scientists determine roughly how many people in the population have already had COVID-19 infections. This information is essential for enabling healthcare professionals to assess our progress toward herd immunity.
Antibody tests are not useful for diagnosing a current infection because the body requires substantial time to build up antibodies. With SARS-CoV-2, data suggest that IgM antibody levels peak about two weeks afterward. IgG antibody levels typically do not peak until three weeks after infection. An antibody test capable of distinguishing between IgM and IgG antibodies can indicate how long ago someone was sick with COVID-19, providing valuable information about the infection phase and potentially helping healthcare professionals refine vaccine priority categories. It could also identify potential donors for convalescent plasma therapy.
Though antibody tests are vital for learning more about COVID-19, they have a few limitations. They may sometimes return false positives or false negatives.
- False positives: False positives occasionally occur when the person has previously had exposure to other coronaviruses, such as those that can cause colds. In that case, the test may detect the antibodies present in the body because of the previous, non-SARS-CoV-2 coronavirus infections.
- False negatives: COVID-19 antibody tests sometimes return false negatives when someone takes the test too soon after infection. Taking an antibody test before antibodies have had sufficient time to build up will return a negative result, even if someone has had an infection.
Scientists are still unsure how long COVID-19 antibodies will protect against the disease, especially as new variants arise. For this reason, the presence of antibodies in a person’s body is not a guarantee of permanent resistance to infection. It does not offer proof of immunity that allows people to resume all usual pre-pandemic activities. Some studies suggest that antibody protection may begin to diminish in as little as two months. However, an antibody test is still an invaluable tool in determining who has had COVID-19 and who has not.
What Is the Rapid Antigen Test?
What are antigen tests for COVID-19? Like the PCR test, the rapid antigen tests are diagnostic. They assess whether the virus is currently in the body. Unlike the PCR test, which detects the virus’ genetic material, the rapid antigen test looks for the virus’ specific proteins or glycans. With the SARS-CoV-2 virus, these are usually the distinctively shaped spike proteins on the virus’ surface.
Purchase Antigen Testing Kits Now
The rapid antigen test generally uses a lateral flow assay for simplicity rather than a more complex CIA or ELISA test. In antigen testing, the person testing the sample mixes it with a solution that denatures any viruses present and frees many of their proteins. The tester then adds the mix to a specialized paper strip that contains an antibody specifically chosen to bind to SARS-CoV-2 proteins. On the strip, a dark or colored band or a fluorescent glow generally appears if binding occurs, indicating the viral proteins’ presence.
What Does an Antigen Test Tell You?
The rapid antigen test for COVID-19 tells you whether you have a COVID-19 infection right now.
If you test positive with the rapid antigen test, you most likely have an active case of COVID-19. False positives are possible, but the most likely scenario is that you have become infected with SARS-CoV-2. Even if you have not been experiencing symptoms, you may be infected or contagious – you may have an asymptomatic infection, or your illness may not have progressed to the point where you begin to show symptoms. A positive antigen test alerts you and the administering healthcare professionals to consider how to treat the present infection.
If you test negative with the rapid antigen test, you most likely do not have an active case of COVID-19. There is a small possibility that you have become infected so recently the test cannot detect the virus, or that the test has returned a false negative for some other collection- or processing-related reason. Still, the most likely scenario is that you are free from illness.
Antigen tests have a few minor drawbacks. They often take longer than other tests for companies to develop because researchers must first identify and produce the antibodies necessary to react with the antigens. They have also tended to lead to a higher false-positive rate than the PCR test, and they can be less sensitive than the PCR test to active infections. For extra peace of mind and clarity, some people choose to get additional PCR testing to confirm their rapid antigen test results.
The rapid antigen test also cannot tell you whether you have had a previous infection. Once an active infection is gone, the antigens on the virus’ surfaces are gone as well.
However, the numerous advantages the rapid antigen test offers makes it a critical tool in the fight against COVID-19. They are relatively inexpensive, so they are widely accessible. They also return results much more rapidly than the PCR — a person can often receive results in as little as 15 minutes. For this reason, they are useful for immediate point-of-care detection and potential at-home use.
Buy Antibody and Antigen Test Kits From SUNLINE Supply
When you need to detect past or current infections, let SUNLINE Supply be your trusted source for COVID-19 test kits. As a company with 24/7 sales availability, we make it our priority to get you the high-quality tests you need as fast as we can. Our competitive prices and bulk availability also mean you can stock up on tests while maintaining a realistic budget that will keep your organization running in challenging times.
Purchase antigen test kits or antibody test kits now, or contact us to learn more.