When to Change Your N95, KN95, or Surgical Masks
Recent supply chain shortages have continued to limit the availability of N95 masks around the country. The healthcare facilities that need them the most, along with construction and other industrial workplaces, still find a shortage of these critical personal protective equipment (PPE) devices. As demand surges, manufacturing bottlenecks keep masks in short supply, making it difficult for many hospitals to maintain a recommended 90-day supply of N95 respirators.
These shortages prompt many workplaces to weigh strategies for conserving their current N95 mask supply. Today, healthcare professionals wear their N95s for much longer than they might otherwise. How long can you wear a disposable mask for? Disposable respirators can be worn for prolonged periods before they become damaged and ill-fitting. However, many factors affect when it’s time to replace your mask.

What Are the Uses of an N95 Mask?
An N95 mask is a class of tight-fitting, seal-forming face covering used in many industries. N95 Filtering Facepiece Respirators (FFRs) are a regulated class of PPE. They include styles such as flat-fold and cup-shaped facepieces. The healthcare sector and other workplaces with respiratory hazards use them to protect workers.
Why are they called N95 masks? The 95 in N95 stands for 95% efficiency. These respirators filter out 95% of airborne 0.3 micron-sized particles. An N99 mask has 99% efficiency, filtering out 99% of these airborne particles. An N100 respirator has 99.97% efficiency, which is virtually 100%. The N means not resistant to oil. Other similar respirators may be listed as R95s, or somewhat resistant to oil, and P95s, or oil proof. R95s and P95s are more likely to be used in industrial settings, such as the oil and gas industry.
The Occupational Safety and Health Administration (OSHA) governs their use for protecting workers. The United States Food and Drug Administration (FDA) regulates their use in healthcare settings. The Centers for Disease Control and Prevention (CDC) provide guidelines for their use in healthcare and other occupations. The National Institute for Occupational Safety and Health (NIOSH), a division of the CDC, approves specific models and manufacturers. NIOSH and independent testing laboratories are responsible for evaluating N95s for performance. They test for:
- Fluid resistance.
- Particulate filtration efficiency.
- Bacterial filtration efficiency.
- Flammability.
- Biocompatibility.
Surgical N95 masks have a different classification from industrial N95s, and it only recently became legal for hospitals to use industrial N95 masks. Besides weeding out viruses, bacteria and mold spores, via a mold mask, N95s filter out hazardous dust like silica and dangerous fumes. As a result, they’re used in many industries, including:
- Manufacturing: Any factory that produces fumes or hazardous dust may require or allow workers to wear N95 masks, depending on the concentrations.
- Oil and gas: Since oil and gas industry workers are often exposed to oil and other respiratory hazards, they are more likely to wear R95 and P95 respirators.
- Construction: Silica dust, released while working with concrete, is a major hazard in construction work. An N95 mask is one option for mitigating respiratory risks on the job. It’s also possible for workers to wear reusable half masks or powered air-purifying respirators (PAPRs).
- Healthcare: Healthcare professionals wear N95 masks when treating patients who may transmit airborne diseases. The masks are worn during interactions with infected individuals and while performing aerosol-generating procedures, such as endotracheal intubation and extubation or noninvasive ventilation.
N95 vs. KN95 vs. Surgical Masks
N95 respirators have several similarities with KN95 and surgical masks. All are used in healthcare settings and share the ability to filter out large droplets. All get evaluated and tested for fluid resistance, filtration efficiency, flammability and biocompatibility by their respective regulators. They’re all considered disposable and aren’t intended to be reused or shared between co-workers. With that, each have have some distinct differences as well.
For comparison, surgical masks:
- Are loose-fitting and allow air to escape around the sides.
- Stop liquids and large droplets from entering the wearer’s mouth and nose.
- Protect the wearer’s saliva and respiratory secretions from reaching others.
- Must be approved by the FDA.
- Do not protect against inhaling small airborne particles.
- Are not considered respiratory protection because they allow leakage around the edge of the mask.
- Are disposable.
Meanwhile, KN95 and N95 respirators are much more similar; but the main difference lies in the certifications.
KN95s:
- Both N95 masks and KN95 masks are made from multiple layers of synthetic material (typically a polypropylene plastic polymer) and are designed to be worn over the mouth and nose. (source)
- Both masks strap behind your ear help to hold the mask in place. (source)
- Both masks must filter out and capture 95 percent of tiny 0.3 micron particles in the air (hence the “95” in the names).Are tighter-fitting and provide a more secure seal around the mouth and nose. (source)
- N95 is the U.S. standard, and the KN95 is the China standard. Because of this, only N95 masks are approved for health-care use in the United States, even though KN95 masks have many of the same protective properties. (source)
N95s:
- Are regulated as N95 Filtering Facepiece Respirators (FFRs).
- Must be evaluated, tested and approved by NIOSH.
- Will allow minimal leakage around the edges of the facepiece.
- Require annual fit testing and medical evaluation for each employee.
- Require the wearer to perform a seal check each time they are donned.
When to Discard an N95, KN95, or Surgical Mask
Under ideal circumstances, outside of supply chain shortages, N95, KN95 and surgical masks get replaced frequently. In healthcare settings, each mask will get discarded after each patient encounter or aerosol-generating procedure. However, in healthcare emergencies, supply shortages may warrant prolonged use or reuse practices.
Many circumstances require a worker to discard an N95, KN95, or surgical mask, regardless of how long it’s been worn. Workers across sectors must dispose of and replace their masks if they:
- Become damaged or deformed.
- Exhibit any nicks, abrasions, cuts or creases in the seal area.
- Have soiled filter material.
- The straps are cut, stretched out or damaged.
- Have a metal nose clip that has fallen off or doesn’t function properly.
- No longer form an effective seal against the face.
- Become wet or dirty.
- Make breathing difficult due to trapped particulates blocking airflow.
- Become contaminated with blood, nasal secretions or other bodily fluids from the wearer or patients.
How Long Can You Wear a Disposable Mask For?
Outside of a respiratory health crisis, any N95, KN95 or disposable surgical mask is meant to be worn only once. In most scenarios, healthcare professionals do not need to wear them for extended periods. Instead, they change them after each patient interaction or aerosol-generating procedure. If the mask or respirator becomes contaminated, or the wearer needs to eat or use the restroom, the N95, KN95, or surgical mask is removed and discarded.
However, in other industries, workers routinely wear N95 respirators, KN95, or surgical masks for several hours at a time. Experience in these industries shows that disposable respirators can maintain their integrity for up to eight hours while functioning within their specifications. This time limit holds for both intermittent and continuous use. However, if the respirator becomes compromised before then, it must be replaced.
During respiratory health emergencies, N95 respirators have had supply shortages. The CDC’s top recommended strategy for managing expected scarcity is employing extended use. Healthcare professionals who work in areas with expected N95 respirator shortages may wear their masks for up to eight hours. Though now, “the CDC has authorized the use of KN95 masks as a suitable alternative to N95 masks for its response to COVID-19.” (source)
While practicing extended use, workers must follow the correct precautions. For example, when wearing the same mask between patients, the worker should only see patients infected by the same pathogen. They must switch respirators when dealing with different pathogens between patients. They should also change masks if it becomes uncomfortable to breathe. Wearing a cleanable face shield can protect the mask’s surface from liquid droplets, helping it last longer. Wearers should treat the masks as contaminated and wash their hands or use hand sanitizer before and after touching them.
Are N95 Masks Reusable at All?
Can you reuse N95 masks? Under normal circumstances, N95 respirators are not reusable. However, severe supply chain shortages cannot be mitigated with CDC-recommended contingency strategies. If supplies become deficient, healthcare facilities may reuse N95 masks under CDC-recommended crisis capacity strategies for limited reuse. Under a limited reuse strategy, the N95 respirator is donned for patient contact, then doffed and stored until the next patient contact.
As disposable respirators, N95 masks have a limit to how often they can be reused. The CDC recommends limiting the number of uses to five per device unless a manufacturer has indicated a particular model can be donned more than five times. As the device is donned, the straps become weaker or stretched, which eventually compromises the face seal. As always, when the respirator becomes soiled, contaminated or damaged, it can’t be reused. If the fit or filtration performance becomes compromised, it also can’t be reused.
The CDC offers two limited reuse strategies. The preferred approach reduces the risk of self-contamination. It involves distributing five N95 respirators to each healthcare staff member who will interact with patients with infectious respiratory diseases. The healthcare worker will wear one respirator each day and store it in a breathable paper bag at the end of each shift. The respirator should be stored for a minimum of five days until its next reuse, allowing pathogens to die off in the meantime.
Decontamination of N95 Masks
If supplies are so limited that a facility cannot distribute five masks per staff member, it can use decontamination. Decontamination reduces the number of pathogens on respirators to allow safer reuse. Decontamination research is still ongoing, and approved methods for decontamination are still being developed. Since N95 respirators are disposable, single-use devices, manufacturers to not authorize decontamination methods for their products.
Third parties, such as decontamination companies, safety organizations and research laboratories, may release decontamination best practices in the absence of manufacturer-approved methods. It’s critical to follow an approved procedure under NIOSH and the FDA’s latest guidelines. Ineffective decontamination can damage a respirator or leave it with active infectious pathogens. NIOSH has identified a few promising methods as of April 2020, including:
- Ultraviolet germicidal irradiation
- Vaporous hydrogen peroxide (VHP)
- Moist heat
Decontamination may damage a respirator’s integrity or fit. This damage comes alongside the deterioration these respirators undergo with prolonged use. Any employer must demonstrate the effectiveness of N95 respirators against the pathogens they’ll encounter after decontamination. Recent studies indicate ultraviolet light and dry heat-treated N95 respirators have seal and fit problems after three decontaminations, allowing for two reuses. VHP-treated respirators showed no deterioration, allowing for reuse up to three times. This treatment is also most effective at viral inactivation with the least impact on filtration efficiency. It is the most promising for respirator decontamination.
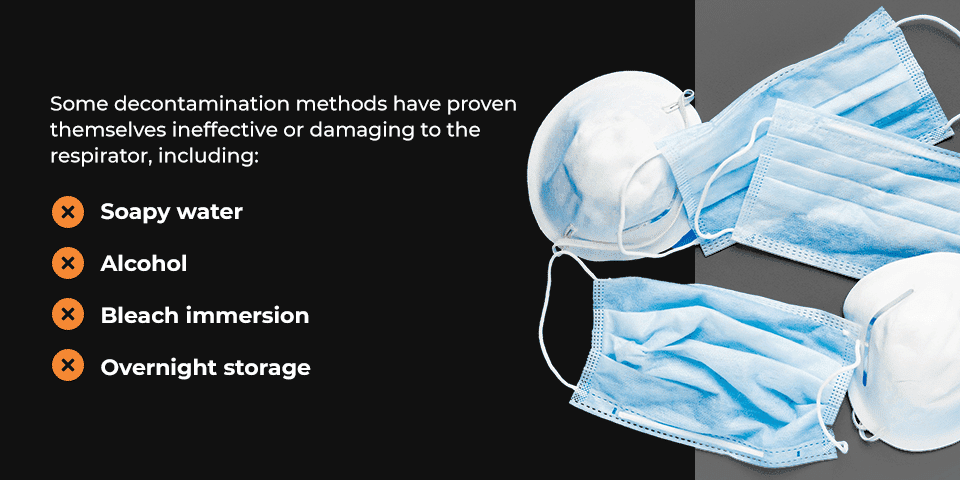
Some decontamination methods have proven themselves ineffective or damaging to the respirator, including:
- Soapy water: Can N95 masks be washed? Disposable respirators cannot be washed with soap and water like a reusable cloth mask. Respirators soaked in soapy water have degraded filtration.
- Alcohol: Isopropyl and ethanol alcohol have both been shown to degrade the filtration efficiency of certain N95 models.
- Bleach immersion: Immersing N95 respirators in a bleach solution degrades their filtration efficiency. However, using bleach-containing wipes can decontaminate several N95 models without causing damage. Bleach residue has health risks, especially for people with asthma. Off-gassing masks for 18 hours in a fume hood can reduce this residue.
- Overnight storage: Since many pathogens, including SARS-CoV-2, remain active on surfaces for several days, overnight storage is not sufficient for decontamination.
Keep in mind decontamination is a last-resort reuse strategy. Other crisis capacity strategies should be implemented first. They include:
- Use respirators beyond their manufacturer-designated shelf life that the CDC has identified as performing adequately in healthcare settings.
- Use non-NIOSH-approved respirators approved in other countries under similar standards.
- Use limited reuse, where the healthcare worker removes the respirator between patients.
- Prioritize N95 respirators and facemasks by activity type, without masking symptomatic patients.
Safety Tips Before Reusing an N95, KN95, or Surgical Mask
Since disposable masks are single-use devices, reusing them presents inherent risks. The most significant risk is self-contamination. When someone, usually the wearer, touches the outer surface of a mask that has been exposed to pathogens, they can then contaminate surfaces or infect others. This may occur while adjusting the mask or unconsciously touching the face, eyes or mask. Another concern is the mask becoming less effective at protecting the wearer after rough handling or excessive reuse.
Because of these risks, extended use is the preferred strategy. Before transitioning to reuse, exhaust other CDC-recommended crisis capacity strategies, like using respirators with approvals comparable to NIOSH standards. When limited reuse becomes necessary, follow these safety tips:
- Wash hands or use a 60% alcohol-based hand sanitizer before and after donning or doffing the respirator.
- Consult with the manufacturer for a recommended maximum number of donnings per device.
- If no manufacturer guidelines are available, limit reuse to five donnings per device and even fewer when decontamination is employed.
- Use a cleanable face shield or a disposable surgical mask over the N95 respirator to protect liquids and large droplets from touching the respirator.
- Hang used respirators in a designated storage area where they will not touch each other, and label them, so the users and last date worn are clearly identified.
- Avoid touching the inside of the respirator.
- Discard the respirator and wash your hands after handling the inner face piece inadvertently.
- Always conduct a seal check upon donning a reused respirator, and do not use a respirator that hasn’t cleared the seal check.
- Always evaluate an N95 mask for proper fit, filtration performance, cleanliness and damage before donning and using it on the job.
- Use clean, non-sterile gloves when donning a used N95 respirator and while performing a seal check, then discard the gloves immediately.
- Since limited reuse of respirators for tuberculosis patients has been an approved practice for decades, prioritize reused masks when caring for these patients first.
- Do not share reused any mask among healthcare professionals.
- Do not wear reused masks between patients infected with different pathogens.
Contact Sunline Supply for Bulk Orders of N95, KN95, and Surgical Masks
Sunline Supply is a company sourcing quality, FDA- and NIOSH-approved PPE products. We’ve been helping businesses like yours combat supply chain shortages by fulfilling bulk PPE orders from reputable manufacturers. We offer N95, KN95, and surgical masks for industrial and healthcare use and can also supply your school or office with PPE appropriate for your workplace. Browse our current N95 respirator inventory, KN95 mask inventory, and surgical mask inventory; and contact us for more details, certifications and informational kits.


